Preventing Cancer: How Sleep Deprivation, Lights and Circadian Disruption Increase Cancer Risk
Dr. Charles A. Lewis © 2016
A Chapter from Dr. Lewis’s book on cancer prevention to be published in 2016
Sleep is essential to health. Lack of, and poor quality, sleep are risk factors for at least several different cancers, including breast, prostate, colorectal and brain cancers.
If lab rats are completely prevented from sleeping, they eat more but lose weight; their heart rates accelerate, and they develop skin ulcers and die within a few weeks. Sleep is required for survival. Even tiny nematodes sleep. If sharks stop swimming, they suffocate. Thus, to keep swimming and keep water moving through their gills, sharks sleep half of their brain at a time. Porpoises also need to come up to the surface to breathe, and birds that migrate long distances across oceans also need to sleep but need to stay awake to survive, so these animals also sleep half of their brain at a time. Although it may seem at times, that some of us are only half awake, this trick does not work in humans; we all need sufficient quality sleep.
Humans sleep about one-third of their life away, or, at least, we are healthiest and perform best when we do. When we have insufficient sleep, reaction times slow, attention lapses, mood becomes labile, cognition foggy, and memory suffers. Decision-making can become faulty, and logic blurred.[1]
Excessive wake-time impairs mood, judgment and reaction time. Nineteen hours of sustained wakefulness is associated with a performance deficit equivalent to a blood alcohol level of 0.05%; the level at which it is illegal to operate a motor vehicle in most jurisdictions around the globe. After 24 hours of sustained wakefulness, the performance deficit is equivalent to a blood alcohol level of 0.1%[2], a level sufficient to impair reaction times and gross motor control.
In addition to the need for sleep, our bodies have circadian cycles that tune the metabolism to daytime activity and nighttime quiescence. These cycles do much more than entrain the sleep cycle to help us wake and sleep coincident to dawn and nightfall. The circadian cycles are intimately tied to the control and release of at least a dozen hormones that control the body’s energy use, activity, appetite, digestion, immune function, growth, renewal, and healing. Disrupting the circadian cycle can throw these hormonal cycles into disarray.
Learning
Sleep provides a quiet and undisturbed space for gleaning and interconnecting the relevant and salient information and processes learned during the day while limiting internal and environmental distractions. The various stages of sleep make different contributions to learning. In the first part of the sleep cycle, SWS (short wave sleep) helps to stabilize visual and declarative memory (“Just the facts, ma’am”). Stage 2 sleep helps reorganize the content that has been learned during the days and helps with learning motor sequencing and automaticity skills such as playing a musical instrument, or coordinated movements such as used in sports, dance or operating machinery. Throughout the night REM (rapid eye movement) sleep enhances the memory, adds insights, explores interrelationships and helps reorganize information into associative networks[3]. These repetitive sleep cycles throughout the night allow for the iterative creation of memory and learning, and for winnowing the salient from the inconsequential. The brain is not relaxing during sleep – it is actively processing information.
One reason the young people require more sleep is that they are more actively learning. Small children take frequent naps that help them learn motor and language skills more quickly. College students often try to learn more information in a sitting than they can organize and understand and much less integrate. Often the information makes more sense in the morning, and sometimes it takes two to three nights sleep for the information to organize into a gestalt. Adults that are actively engaged in learning have creative demands or require peak attention and reaction times need to dedicate eight hours a day to sleep.
Recovery and Detoxification
Chronic sleep deprivation usually only causes a mild decline in subjective functioning. Nevertheless, it can cause a severe decline in attention and reaction times. When people are severely and chronically sleep deprived, they do not feel much worse than if they were only mildly sleep deprived, however; their functioning can be seriously impaired. Maintenance of peak reaction times requires just over eight hours of sleep each night.
Many adults make do with much less sleep time without obvious problems. Even if sleep is restricted to only 4 hours a night, most adults will not complain of feeling fatigued or impaired even after two weeks of curtailed sleep. It appears that there are different thresholds for feeling sleep deprived for different individuals[4]. Nonetheless, those who feel well when sleep is limited are not unimpaired by sleep deprivation; rather they just don’t feel tired. They still suffer just as severe performance deficits as those who do feel tired.
Peak functioning, as measured by attention measurements, actually does not depend not on sleep, but rather, on avoiding excessive wakefulness. Being awake too long diminishes focus. The effect of time awake is cumulative; being awake an additional hour each day for 8 days in a row diminished the level of focus and attention equivalent to missing one night’s sleep; staying awake one extra hour daily for 16 days in a row will cause the difficulty in focus and attention that missing two night’ sleep would. Performing at full attention and focus proscribes being awake no more than about 16 hours per day on average[5]; resulting in the need for about 8 hours of sleep.
Excitatory neurotransmitters, such as glutamate, associated with activity and alertness, are neurotoxic; when they accumulate, they can damage the brain. Sleep provides an opportunity for the brain to detoxify, replenish antioxidants and repair itself. During sleep, the glymphatic system flushes wastes from the cerebral spinal fluid more quickly to help recover from the toxins and metabolites that accumulate during wakefulness.[6]
Sleep deprivation also impairs mitochondrial health. Deprivation of REM sleep can induce loss of neuronal mitochondria through mitophagy[7], a process in which the mitochondria, the energy production units of the cell, self-destruct. The CLOCK gene, which helps regulate circadian cycles, is involved in the growth and repair of muscles[8].
Several of the genes involved in energy metabolism and for encoding antioxidant proteins have increased transcription during sleep[9]. During sleep, an accounting of energy utilization and oxidative stress is made, and the results are used to plan and accommodate the next day’s needs for energy and need for antioxidants. Energy accommodation is provided by control of thyroid and hormones to fine tune the metabolic rate, and by hormones that control the appetite. Sleep deprivation increases appetite. Melatonin, released from the pineal gland not only helps induce and maintain sleep but also is an important antioxidant that helps protect neurons in the central and in gastrointestinal, nervous systems. Melatonin is a non-recyclable antioxidant for the nervous system; oxidized melatonin acts as a signal, which through the Nrf2, NF-κB, and AP-1 pathways, increases the antioxidant response element (ARE) and other proteins that provide protection from endogenous and xenobiotic toxins and oxidative damage.[10] ARE proteins protect the cell from damage and protect the body from cancer.
Inflammation and Immunity
Sleep deprivation promotes inflammation. It causes increased levels of C-reactive protein, and of the cytokines IL-1β, IL-6, and IL-17. These cytokines are signals for inflammation. The changes in the appetite hormones; leptin and ghrelin, observed in sleep deprivation may be the result of changes in these cytokines. IL-6 is usually found to be elevated fibromyalgia syndrome, a condition in which non-restorative sleep is common. The risk of heart disease is elevated in short-sleepers because of inflammation. There is also an increased risk of dysrhythmias caused by increased adrenergic activity. IL-6 decreases SWS and causes fatigue[11].
Sleep and circadian rhythms have a critical role in the development of immune function. The ROR (retinol-related orphan receptor) genes, which are subject to circadian influence, impact the differentiation of T helper cells into different lineages. Different types of T Helper cells are used by the immune system to focus on specific targets, such as different types of infections or tumor cells. Sleep deprivation or disruption of the circadian cycle shifts T helper cell development towards TH17 cell development. TH17 cells are involved in the chronic inflammatory and autoimmune diseases including multiple sclerosis, rheumatoid arthritis, systemic lupus, inflammatory bowel disease, psoriasis, and asthma.[12] TH17 cells underlie the development of entero-immunopathies; dysfunctional food sensitivities. Thus, sleep deprivation may cause the developing food sensitivities that cause migraine, irritable bowel syndrome, depression and other maladies. Sleep deprivation is also associated with an elevated B lymphocyte and lower NK-cell populations, thus affecting the body’s immune response to infection and injury.
The immune system does not like to fight two battles on different fronts. When it is diverted, and dedicating its resources to TH17 cell immune functions, the immune defenses against cancer and other threats is compromised.
Table 1: Effects of Sleep Restriction on Hormones[13] and Cytokines[14]
Hormone |
Effect of Sleep Deprivation |
Effect on Health |
Leptin(Satiation hormone) |
Lower circadian peak leptin levels. Lower daily leptin production. Likely drives thyroid control (TRH). |
Lower levels cause increased hunger, especially for high caloric, soft, palatable foods |
(Acyl)-Ghrelin (Hunger hormone) |
Increased in short sleepers[15] |
Stimulates hunger |
Orexin (Hypocretin) |
Increased in sleep deprivation. |
Increases activity |
TSH (Thyroid Stimulating Hormone ) |
Loss of circadian nighttime peak.Lower TSH output. |
Fatigue and lowered energy use |
Cortisol |
Decreases circadian cyclic variation. Increase daytime and total cortisol output. |
Increased abdominal obesity. |
Sympathovagal balance |
Increased sympathetic activity. |
Increased resting heart rate, blood pressure, and risk for arrhythmia. |
Insulin |
Decreased glucose tolerance.Decreased insulin sensitivity. |
Increased risk for Type 2 diabetes. |
IGF-1[16] |
Decreased production. |
Decreased healing, increased mortality[17] |
Interleukin-6[18] (IL-6) |
Proinflammatory cytokine; increased in sleep deprivationMay decrease leptin output. |
Chronic inflammation |
Interleukin-1β (IL-1 β) |
Proinflammatory cytokine |
Chronic inflammation, increased TH17 immune function, decreased TH1. |
Interleukin-17 (IL-17) |
Proinflammatory cytokine; favors TH17 immune function. |
Chronic inflammation, enteroimmune disease. |
C-Reactive Protein |
An inflammatory marker associated with risk of coronary artery disease. |
Increased risk of coronary artery disease. |
Melatonin |
Decreased output. Melatonin is an antioxidant for the nervous system. It stimulates T4 and T8 lymphocyte production.[19] Helps with memory consolidation. |
Decreased T-cell immune function. Impaired memory consolidation |
Energy Balance
Individuals who sleep fewer hours are more likely to become obese. Children who sleep less than ten hours a day are eighty-nine percent more likely to be obese than children who get more sleep, and adults who get less than six hours sleep are about fifty-five percent more likely to be obese than adults who get more than six hours of sleep[20]. This association of short sleep time with obesity has been found in more than 30 studies performed on six continents; this effect is not limited to North American or to the Western lifestyle.
Obesity is also associated with longer sleep time; obesity greatly increases the propensity to snore. When snoring becomes severe, it is often associated with sleep apnea, where the person’s breathing becomes obstructed momentarily, and sleep is disturbed. Heavy snorers with sleep apnea may experience dozens of semi-awakenings throughout the night but have no recollection of them. These frequent arousals result in poor quality, non-restorative sleep as the sleeper spends little time in deep, restorative, Stage 2, SWS and REM sleep. Thus, although patients with sleep apnea may spend more time in bed and more time sleeping, they can still have large sleep deficits and feel sleepy and fatigues during the day. In a vicious cycle, the sleep deficits from sleep apnea promote an increase in appetite, further obesity, worsened snoring and worsened apnea and sleep deficits.
Obviously, a lack of sleep leads to fatigue. It is not only the lack of sleep, especially short wave sleep, but disruption of the diurnal cycle of thyroid hormones, growth hormone, and cortisol, and the increase in inflammatory cytokines that cause fatigue. The fatigue, lack of energy and decrease in muscle function act to dissuades many short sleepers from robust exercise.
A Setup
Yes, this has been a setup. Obesity, lack of exercise, oxidative injury, inflammation, with a decline T-cell function, the immune cells most closely linked to targeting cancer cells; all of these are risk factors for cancer. Put these together, and you begin a good tally of cancer risk factors.
In a study sampling two million people enrolled in the Taiwanese national health insurance program, sleep disorders were associated with a seventy percent increased risk of cancer. Individuals with obstructive sleep apnea (OSA) had a greater than doubling in the hazard for breast, kidney, bladder, and thyroid cancer. Suffering from OSA was associated with 3.69 times higher hazard of prostate cancer. The risk of prostatic hypertrophy is also elevated among men with sleep apnea.[21] Colorectal cancers were increased by 55 percent in persons with OSA. Cancer risk was similarly elevated among those with chronic insomnia or parasomnias.[22]
(Parasomnias are abnormal movements, behaviors, emotions, perceptions, and dreams that occur while falling asleep or during sleep. They usually involve a state of partial arousal. They include sleep walking, teeth grinding, night terrors, and restless leg syndrome.)
Another study found that OSA was associated with a doubling of breast cancer incidence among women aged 30 to 59 and a tripling of incidence among women over sixty.[23] The risk of primary brain cancers has also been found to be raised by seventy percent among persons with sleep apnea.[24]
Shift Workers
Shift work has been found to be associated with increased risk of cancer. A meta-analysis of 25 studies has shown a 48 percent increase risk of breast cancer among women who do night/shift work, especially in women who do it for 20 years or more.[25] Doing three of more nights of shift work a month was sufficient in increase breast cancer risk among nurses.[26] Night shift work raises the risk of breast cancer by about three percent for every five years of exposure.[27] The risk is potent enough that women who have been diagnosed with breast cancer are advised not to do night shift work.[28] The increased risk of prostate cancer from night shift work is similar to that for breast cancer; 2.8 percent increase in risk for every five years of exposure.[29]
Night shift work has also been found to be associated with an increased risk of colorectal cancer; here the risk is considerably higher, with an 11 percent increase in risk for every five years of shift work.[30] The risk of colorectal cancers may be especially elevated in night shift workers because of its disruptive influence on the circadian cycle of the intestines.
The motility of the gastrointestinal system is mediated by CLOCK genes expressed in intestinal epithelial cells and in neurons in the enteric nervous system which help control circadian rhythms.[31] (Yes, the gastrointestinal system has its own brain). Gastric emptying times are longer for solid foods in the evening than in the morning. The propagation of contractions in the small intestine is slower at night; moving only about 2.9 cm/minute, as compared to 6.4 cm/minute during the day.[32] Colonic motility is low at night but increases in the morning, aiding in defecation. Melatonin increases blood flow and acts as an antioxidant[33] that protects the enteric nervous system. Disruption of the circadian cycle by alterations in sleep time and meal times can provoke changes in GI motility. Disruption of circadian rhythms, such as occurs with shift work or time zone traveling, can lead to gastrointestinal symptoms including bloating, abdominal pain, diarrhea, or constipation19.
Disruption of the circadian cycle can cause intestinal dysmotility. Irritable bowel syndrome and gastrointestinal reflux are associated with sleep disorders and common among shift workers. Nurses on rotating shifts are twice as likely to have a functional bowel disorder as those working day shifts[34]. Missing meals during the day or feeding at night may also disrupt gastrointestinal circadian cycles[35], [36].
Glucose, insulin, ghrelin, leptin, and GLP-1 levels follow meal patterns.[37] Nighttime eating can offset the intestinal circadian rhythm, and nighttime meals result in increase blood sugar and triglyceride levels, compared to the same meal consumed during the day[38]. In addition to cancer, shift workers are at increased risk of obesity and cardiometabolic disease.[39] Disruption of the circadian cycle causes changes in appetite that increase risk for obesity.[40] Shift work also results in elevated triglyceride levels, increased BMI, waist circumference and obesity, and blunted response to insulin.[41] Indeed, circadian disruption in shift workers increases the risk for metabolic syndrome, diabetes, depression, cardiovascular disease, premature aging, and cognitive impairment, in addition to the increased risk of cancer. [42] [43]
Waiters have also been found to be at increased risk of cancer. The availability of alcohol and exposure to secondhand cigarette smoke may partially explain this risk. Perhaps in an attempt to help induce sleep, it has been found that shift workers, especially younger men doing shift work, are more likely to binge drink than their not shift working peers.[44] Night workers also tend to smoke more[45] and to eat foods associated with inflammation.
In addition to women with breast cancer, I recommend that women at high risk for breast cancer, such as those with high-risk BRCA alleles, with a strong family history of breast cancer, or with other breast cancer should also avoid night shift work. Since night shift work is also a strong risk factor for colorectal cancer, those with a family history of colorectal cancer should also avoid night shift work.
Melatonin
Melatonin is a multifunctional substance produced in the body from the neurotransmitter serotonin. Melatonin is a hormone that helps with sleep but is also an important antioxidant for the central, autonomic and enteric nervous systems. The pineal gland, located deep within the brain releases melatonin when the level of light reaching the retina of the eye is low. Exposure to light at night disrupts melatonin production. Light exposure and melatonin disruption are designated as by the World Health Organization as a probable human carcinogen.
Melatonin inhibits human breast cancer cells that are stimulated by estrogen, decreasing estrogen-induced gene transcription.[46] Melatonin also prevents the uptake of linoleic acid (LA), a fatty acid the support tumor growth by breast cancer cells. LA is converted to 13-HODE, which amplifies the activity of the EGF MAPK pathway that leading to cell proliferation.[47] This is especially relevant for 70 percent of breast cancers that are estrogen receptor alpha (ERα) positive. Light at night induces disruptions in the circadian rhythm and output of melatonin. This, at least in part, explains the increased risk of breast cancer in shift workers.[48]
Over 30 percent of women with ERα-positive (ERα+) breast cancer are intrinsically resistance to tamoxifen and similar anti-estrogenic medications used in the treatment of breast cancer. Eventually, most breast cancer patients develop resistance to these medications. In animals implanted with ERα+ human breast cancer cells, light-induced melatonin disruption increased tumor growths and conferred resistance to tamoxifen treatment. In animals exposed to dim light at night and given melatonin did not become resistance to tamoxifen. Supplementation with melatonin was able to re-established the sensitivity of ERα+ breast tumors to tamoxifen and promoted tumor regression in these animals.[49] In another, quite ingenious approach, human ERα+ breast tumors implanted into rats was perfused with blood from healthy women. When this blood was drawn from women during the day time or at night after exposure to fluorescent lighting, it increased tumor metabolism. Blood drawn at night from women during darkness decreased tumor energy use lowering cAMP by 86%, and decreased tumor DNA content by about 70 percent. However, blocking melatonin allowed the tumor activity that had been inhibited by the dark-night blood from women.[50]
Women with ERα+ breast cancer should not do shift work as there is substantial evidence that it promotes tumor growth and promotes resistance to anti-estrogen therapy. Additionally, these women should carefully avoid light during their sleep cycle.
The circadian drive is most sensitive to blue light with peak sensitivity to light at wavelengths about 450 nm. Low light in this region of the spectrum helps calm get us in the mood for sleep. Melatonin suppression appears to result from non-image forming retinal cells containing the pigment melanopsin.[51] Melanopsin has its peak sensitivity to light with a wavelength around 500 nm but is stimulated by a broad range of the spectrum, from blue to yellow. Melanopsin has little sensitivity to red light, above 600 nm. Although blue light around 450 nm stimulates wakefulness and helps entrain the circadian cycle, and melanopsin activation by light suppresses melatonin, these are separate, complementary pathways. The amount of light required to suppress melatonin output is much lower than the amount of light that stimulates attention and wakefulness.
It takes very little light to disrupt melatonin output. Light at 0.25 lux, the amount of light the leaks under a closed door into a dark room, or the amount transmitted through the closed eyelid from a television in the room is enough to lower melatonin output.[52] If you can see color in your environment or have enough light to read letters smaller than several inches high, it is bright enough to suppress melatonin output. Anyone who has tried to sleep out of doors on clear full moon night knows that it is bright enough to disturb sleep. Light on an average night, away from artificial lighting is not.
Women who do shift work can use melatonin at bedtime. This may mitigate cancer risk caused by circadian disruption. The use of low dose melatonin is considered to be essentially risk-free.[53] Women with ERα+ breast cancer should discuss the use of melatonin with their physician, especially they are using tamoxifen or similar medications, or if they have failed to respond to it.
Melatonin also suppresses prostate cancer growth. Sleeping in the dark suppresses prostate cancer proliferation, at least in lab rats. Additionally, exposure to bright light during the day, especially light in the blue range, increases mid-dark cycle the output of melatonin by several times. Exposure to bright daylight increased nighttime melatonin output and was found to delay the development of human prostate cancer xenografts in rats, and slow the cancer growth and metabolism.[54] Underexposure to sunlight during the day, and over exposure to light in the evening and during sleep at night promotes cancer growth.
Getting exposure to midday sunshine also creates vitamin D3 in the skin. There are ROR and RZR receptors in the pineal gland that help mediate melatonin production as well as other proteins that are involved with sleep.[55] Vitamin D is a ligand for the ROR and RZR receptors[56], and thus, vitamin D made in the skin during the day by sunlight may help with the production of melatonin and with other aspects of the circadian cycle. Vitamin D’s effect on the pineal gland may partly explain why sunshine makes us feel good.
Vitamin D may be helpful in the primary and secondary prevention of circadian and other sleep disorders25. If vitamin D supplements are taken, midday is likely the most advantageous time.
Vitamin B12 amplifies the response of light in resetting the circadian clock[57] and is helpful for some individuals with circadian rhythm disorders[58]. Vitamin B12 levels should be checked when investigating sleep disturbances and in patients with cancer. The vitamin B12 level should be maintained between 500 and 900 pg/mL.
I’m Only Sleeping
Whether studying Americans, Europeans or Asians, the lowest mortality rates, when assessed by daily sleep duration, are between six and eight hours per night[59],[60],[61],[62],[63]. Sleeping less than six hours is associated with a slight increase in mortality, and more than nine hours of sleep at night is associated with an even higher risk. The reason that more sleep is associated with higher risk of mortality among adults probably results from the reasons they need more time to sleep; because their sleep is of low quality or fractured. Retired persons tend to sleep more, perhaps because of less demanding schedules, but this may also be due to poorer health. Even after adjusting for multiple risk factors, five hours of sleep in men and six hours for women appears to be sufficient to prevent an increased risk of mortality when compared to seven or eight hours. Less than four hours of sleep is a risk factor for higher mortality, similar in magnitude to the risk of nine hours.
The optimal sleep time for adults appears to be about 7 hours and 45 minutes. This is about the length of time that adults will sleep if they have no impediments to sleep; a quiet, dark place, no appointments, no scheduling imperatives, no night-time disturbances. Most people take another 15 minutes to falling asleep and spend 15 minutes lying awake in the morning before arising. This is nearly exactly the 7.7 hours average sleep time, and 8.3 hours average time in bed observed in studies of healthy Americans.
Restoring Circadian Rhythm
Keeping regular meal times helps maintain the gastrointestinal circadian rhythm and helps with regular sleep. This is especially important in small children. Avoid large meals within 3 hours of bedtime. A protein/ carbohydrate/calcium snack, ice-cream for an example, an hour before bedtime can induce production of serotonin and melatonin, and help with sleep onset.
Adhering to a regular wake and rise time is fundamental to improving nocturnal sleep efficiency and daytime alertness
Low dose melatonin (0.3 to 0.5 mg) given several hours prior to sleep has been found helpful to restore circadian rhythms. Low-dose melatonin has also been found to be helpful in preventing “sun-downing” delirium in the elderly[64]. Larger doses of slow-release melatonin (3 mg to 6 mg) may be helpful for maintaining sleep in patients with early morning wakening. The underlying cause of the sleep disturbance should be investigated and treated.
As a natural product, present in animals and some plants, melatonin is sold a food supplement. Endogenous production of melatonin requires serotonin and the B6 vitamin, pyridoxine-5-phosphate. Most people have adequate B6 vitamin levels, but low levels are associated with increased risk of colon cancer.[65]
Between 0.3 and 1.0 mg of rapidly absorbed, sublingual melatonin at bedtime is a reasonable dose to promote the onset of sleep. Up to 6 mg, usually in slow release form, may be used to maintain sleep, although 1.5 mg is sufficient for most people.
Melatonin is useful in the treatment of many entero-immune and inflammatory diseases including metabolic syndrome[66], fibromyalgia, IBS[67], GERD[68], migraine[69], cluster headaches[70] and protects against Alzheimer’s disease and depression[71].
Having adequate vitamin B12 levels is important for a full circadian response to light. Vegan diets do not contain vitamin B12. People with dry mouth and those with poor dentition that do not chew meat well enough to mix it with saliva can have low B12 absorption. Haptocorrin, a protein present in saliva, protects vitamin B12 in the diet from destruction by stomach acid. For those needing an oral supplement, sucking on a B12 tablet to mix it with saliva increases the amount that can be absorbed by over 100 times. Individuals with sleep disturbances and those with cancer should be tested to make sure vitamin B12 levels are adequate. Supplementation should be used to maintain vitamin B12 levels between 500 and 900 pg/ml.
Vitamin D3 level should also be tested in individuals with sleep disturbances and in cancer patients. Vitamin D3 levels optimal for cancer prevention are over 90 nmol/L (36 ng/ml) of 25OHD3, and perhaps as high as 120 nmol/L (48 ng/ml). A dose of 2000 IU of vitamin D3 daily is sufficient to raise 25OHD3 above this 90 nmol/L in most adults.[72] Low vitamin D levels may also cause the parasomnia, Restless Leg Syndrome (RLS). Normalizing vitamin D level has been found to improve symptoms in RLS patients that have low vitamin D levels.[73]
Vitamin D2, from mushrooms and synthetic vitamins, does not prevent cancer.[74] Note: The strongest effect of vitamin D on cancer mortality has been seen in studies with follow-up greater than 5 years.65 In some studies, vitamin D3 levels were not associated with a change in cancer incidence but were associated with a decrease in cancer and overall mortality. This suggests that vitamin D may slow cancer growth.[75]
Low iron levels are associated with sleep disturbances and iron deficiency, and associated sleep and cognitive problems are common in children.[76] Sleep disturbances in children with autism improved after correction of the iron deficiency[77]. Iron deficiency also affects sleep in adults. In a study of patients with anemia, heart failure, and sleep disturbances, treatment for anemia including iron not only improved heart function but also caused improvements in sleep deprivation and improved both central and obstructive sleep apnea[78]. Iron deficiency is associated with RLS, difficulty falling asleep and daytime fatigue.[79] Iron deficiency not severe enough to manifest as anemia can still be severe enough to cause delays in neurodevelopmental milestones[80], thus sleep disturbances in infants and young children should be investigated with blood tests for ferritin. Testing for anemia is not adequately sensitive to rule out iron deficiency severe enough to cause sleep disturbances.
Caution: Most studies vitamin supplement use show an increased risk of cancer for adults taking them. High levels of some B vitamins can increase the risk of DNA breaks and many vitamins and mineral supplements increase cancer growth. The supplements mentioned in this chapter should be only used to raise vitamin levels to correct deficiencies and bring levels to their optimal for metabolic function. While vitamin D levels below 200 nmol/L are probably not associated with increased risk, both vitamin B6 and B12, mentioned in this chapter have U-shaped curves for risk, with increased cancer risk at both low and very high levels.[81] The best source of vitamin B6 is a healthy diet. Most American adults do not get enough sunlight to form sufficient vitamin D, and thus, most benefit from vitaminD3 supplements. Vitamin B12 inadequacy is common in vegans and in people with problems absorbing the vitamin, which is common in the elderly.
Getting Better Sleep
Fatigue is no fun. Sleep disturbances, such as sleep apnea, are medical conditions and need to be treated. Most sleeping medications, however, do not restore normal sleep cycles and should be avoided. If an adult dedicates eight hours to their pillow and still does not get sufficient quality sleep to wake feeling refreshed, there is a problem that should be addressed.
Waking in the wee hours of the night with worries and ruminations is a common sign of depression. These symptoms recover with treatment. Snoring and OSA should be treated early to prevent fibrosis of the muscles of the throat that worsen this condition.
ADHD (Attention Deficit Hyperactivity Disorder) should be assumed to be a sleep disorder or secondary to sleep deprivation until proven otherwise. At least 50% of children with ADHD have sleep disorders; it is safe to assume that sleep deprivation causes a similar effect on college students and adults. For children, just adhering to a calm evening and bedtime routine, lowering of the lights and avoidance electronic screens in the evening, and a routine of tooth brushing, a warm bath, a story and a set bedtime with lights out, helps get kids to bed and often improves the symptoms of ADHD.
Exercise: Getting sufficient physical activity during the day helps with sleep. Part of this may be the brief rise and subsequent lowering of IL-6 levels that occur with exercise. Exercise helps improve sleep efficiency and decreases sleep fragmentation in the elderly.415 Vigorous or strenuous exercise, however, should be completed several hours before regular sleep time as it stimulates wakefulness.
Obesity: Sleep deprivation is an important cause of obesity. Obesity increases the risk of snoring and sleep apnea, and thus can worsen the sleep disorder. Treatment of other contributing factors of obesity can also be treated to help break the loop of obesity and sleep deprivation.
Avoid Stimulants: Coffee is a health food for most people that, among other things, stimulates the production of antioxidant enzymes and lowers cancer risk. Studies of moderate coffee intake show that coffee drinkers are less depressed, more active and live longer. Moderate amounts of caffeine (200 to 400 mg per day) are associated with longevity and health (about 2 to 5 cups of coffee a day). Caffeine is the world’s favorite stimulant; it is used to ward off sleep.
Our bodies have two sleep drivers, the homeostatic drive that makes us sleepy after we have been awake so many hours, and the circadian drive that responds to daylight. Adenosine is a metabolite that makes us feel tired, and an important part of the homeostatic sleep drive. Adenosine builds up during wakefulness and is eliminated during sleep. Caffeine blocks the adenosine receptors in the brain, and thus, enhances wakefulness. Caffeine does not work against the circadian sleep drive. When used in the morning or early enough in the day, caffeine can be used to enhance the homeostatic diurnal drive by helping to time activities to the desired alert-awake/ drowsy-sleep cycle. Used inappropriately, caffeine is a major cause of insomnia.
Caffeine consumed in the morning is rarely a problem for night sleepers. But it should not be used less than about six hours before bedtime to prevent it from disturbing sleep. Caffeine in the evening is more likely to cause stomach upset. Irritability, fatigue, depression and heart arrhythmias may be associated with disturbed sleep caused by caffeine rather than by caffeine itself. The average half-life of caffeine in the body is about 6 hours. If two cups of coffee are consumed after supper at 7 PM, 63 percent of the caffeine would still present in the system at 11 PM. Persons that metabolizes caffeine more slowly than average take longer to eliminate caffeine, and may even have trouble sleeping if coffee is consumed in the late afternoon.
Caffeine causes habituation and can be associated with headaches if a dose is late or missed. To alter a coffee habit, wean the dose slowly over several days.
|
Chocolate contains some caffeine, but much less than coffee. Chocolate also contains the alkaloid theobromine, a molecule very similar to caffeine, but at a level several times higher than its caffeine content. Like caffeine, theobromine binds to adenosine receptors and thus promotes wakefulness and can cause insomnia. Caffeine is, in part, metabolized into theobromine. Theobromine has a seven-hour half-life for most individuals. Although less active, theobromine also blocks adenosine and the homeostatic sleep drive. Chocolate can cause insomnia when large amounts are consumed late in the day. |
Avoid Nicotine: Banish tobacco. Not only is it a highly addictive and carcinogenic, but it is also a stimulant that can disturb sleep. Nicotine can reset the circadian clock to the wrong time.
Avoid Alcohol: Although alcohol is often used to self-medicate to help initiate sleep, it is not an effective agent for treating insomnia. Alcohol use decreases deep restorative sleep stages and causes fragmentation of rapid eye movement (REM) sleep. Alcohol consumption desynchronizes circadian rhythms, thus making regular sleep more difficult[82]. Alcohol also prevents light from resetting the circadian clock[83]. This adds to the risk of breast cancer caused by alcohol.
When the alcohol begins to wear off, glutamine levels in the brain rebound and acts as a stimulant, causing shallow, non-restorative sleep or wakefulness. Alcohol also blocks vasopressin production in the pituitary, leading to increases urine output, promoting nocturia (nighttime urination), sweating, dehydration, and dry mouth. Alcohol depletes glycogen stores in the liver, briefly raising blood sugar, followed by a fall in blood sugar and causes fatigue. Once habituated to alcohol, stopping its consumption can temporarily induce insomnia and nightmares, deterring efforts to avoid it. Alcohol should be avoided for at least 3 hours before expected sleep time.
Stress Relief: Stress can disrupt circadian hormonal rhythms, and the disruption may continue long after the original stressor is no longer present.[84] Disturbances in the circadian cycle can cause sleep deprivation and poor response to stress. Stressor should be identified and eliminated, or accommodated.
Don’t fret: Wanting to fall asleep not only makes it harder to fall asleep but also increases the chances of wakening during sleep and increases sleep fragmentation[85]. If unable to sleep, just relaxing in a dark, comfortable environment provides benefit. Meditate on things that make you happy.
Create a Restful Sleep Environment: The purchase of a well-made, new car, with proper maintenance, care and luck should provide about 4000 hours of service; 4000 hours at an average of 50 MPH gives 200,000 miles, costing about $25 per hour, accounting for typical expenses. A good mattress provides about 30,000 hours of comfortable service at a cost of about six cents an hour. A comfortable bed is an inexpensive luxury and investment in health and productivity.
Make sure your bed is comfortable, and service it frequently (Turn mattress according to the manufacturer’s instructions, e.g., twice a year). Get comfortable, sheets and pillows and replace them when they are worn out. Pilled sheets are irritating, and old pillows are uncomfortable and downright nasty. Doctor’s orders; replace them. Polyester pillows should be washed every three months and replaced after six to nine months. Memory foam pillows can last from 18 months to three years.
To help promote sleep, the temperature of the bedroom should pleasant and cooler than the daytime room temperature. The room should be dark, and quiet, without distractions. There should not be a TV or computer in the bedroom; reserve those distractions for a different location.
Additionally, the bedroom should be dark for sleep.
Darkness and Light: Exposure to bright light at in the evening and night disrupt the circadian clock through its effect on the circadian sleep driver.
Fluorescent and LED lights have more energy in the blue end of the spectrum than the incandescent lights, and it is this blue light that most potently disrupts the circadian rhythm. Fluorescent light is used in most workplaces and now are used in the home. In the workplace, it decreases fatigue and increases productivity. In the home, it is used to save energy. Thus, in recent years, household lighting has a greater negative impact on the circadian drive in the hours before bedtime than in the past when incandescent lights were the norm. Use of computer monitors, tablets, phones and televisions adds to the exposure of blue light on the retina in the evening hours.
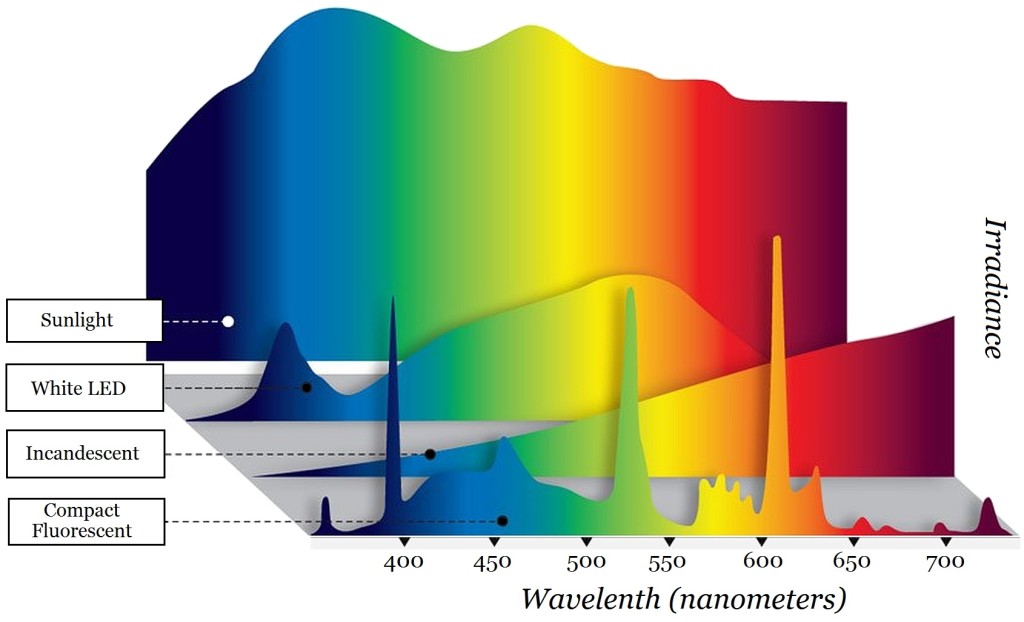
The image above shows the spectral output of sunlight, as well white LED, incandescent, and fluorescent lights used in the home. Commercial fluorescent tubes have an even larger peak in the blue spectrum than do compact fluorescent lights (CFL).
Notice in the image that the sunlight has a large cutoff at the violet end of the spectrum; this is UV light, which the human eye cannot see, but which causes the formation of vitamin D3 in the skin, and sunburn and skin cancer with excessive exposure. There is also a large cutoff apparent for the invisible infrared light from sunlight and incandescent lights. Some infrared light is felt as heat. For the incandescent light, 90 percent of the energy is wasted as infrared light and heat, and thus, these lights have poor energy efficiency.
Standard white LED lights and fluorescent lights are made by having a blue or UV light excite phosphors that glow in the green to red area of the spectrum, so that when combined, they give a white light. Depending on the mix of phosphors, the light can be daylight (bluish), or have warmer colors with more red light from the red end of the spectrum. Alternatively, LED’s can create white light by mixing colored LED’s, typically blue, green and red.
A problem with most white LED and all fluorescent lights is that the peak of light in the blue spectrum keeps us awake. Incandescent lights are being phased out in the U.S. to improve energy efficiency. As can be seen in the illustration, incandescent lights have a much less light in the blue area of the spectrum and have much less effect on delaying sleep. When children are exposed to the fluorescent and standard white LED lights in the evening, it is much more difficult to get them to settle down and go to sleep in the evenings. LED’s can be made with dimmable blue content or with much lower amounts of blue light, but these are not ones typically sold in stores.
The problem with blue light in our homes in the evening is not limited to light fixtures. Televisions, computers, and phones also have high levels of light that impede the onset of sleep.
Even electronic paper readers project a great deal more blue light into the eye than is encountered reading a paper book with room light. Like to read a few pages of a book before falling asleep? Reading an ebook around bedtime reduces sleepiness, increases the time to fall asleep, decreases melatonin output, and reduces next-morning alertness compared to reading a printed book.[86] Computer monitors are problematic because of their close viewing, and the televisions are increasing in size. This should be expected to raise the incidence of sleep and circadian disturbance and their associated disorders which include mood disorders, ADHD, bipolar syndrome, premenstrual dysphoric disorder, and cancer.
Yellow or amber tinted glasses worn in the evenings or night help prevent disturbing the circadian cycle and diminish the decline in melatonin output.[87] They are known as blue-blocking glasses. Yellow (not dark amber) glasses are also helpful for reducing glare when driving at nights.
Computer apps are available that automatically change the screen to a “bedtime mode” by diminishing blue light from the monitor at a set time in the evening.[88] These can help decrease the effect computers and phones have on delaying sleep. LED lights can be made to diminish the blue content in the evening hours, or made with less blue light content.
Lighting in a “smart home” could shift lighting to lessen the sleep delay caused by blue light. Lighting at around 200 lux with attenuated blue light that still appears white was found to only lower melatonin 6% more than 3 lux light. This lighting would not be appropriate for most work settings, as there was a decrease in alertness77, but is would be appropriate for home use in the evening, and help get the kids calmed down for bed.
Bright light in the mornings and the use of “natural sunrise” can be used to entrain the circadian clock. “Alarm clocks” are available that gently increase light in the room, simulating a natural sunrise.
For sleep, the bedroom should be very dark to permit adequate melatonin production. If the bedroom windows let in excessive light from streetlights or other light pollution at night, blackout or other light impervious blinds are recommended. Aluminum blinds block light well, whereas plastic ones do not. There should be no more light in the bedroom at night than what is required to see large shapes after the eyes are adjusted to the dark.
To avoid blocking nighttime melatonin production, the bathroom should be equipped with a light, for use when getting up at night, that when illuminated allows safe use of the toilet and sink. A dim orange or red LED light, bright enough to use the facilities, with a peak output at 650 nm, should not melatonin output. A dim red LED in a smoke detector should not be a problem in the bedroom.
Napping: Snatching a siesta can help one catch up from a sleep deficit. Napping has anti-inflammatory effects; helping to decrease the level of inflammatory IL-6[89]. Napping is a healthy activity for adults, and can be used to increase performance and learning. Naps are an effective sleep supplement that increases vigor and alertness, decrease information overload and boost mental performance and memory.
Table 2: Nap Guide
| 6 to 30 minutes
Stage 2 Sleep |
Quick refresher. Avoids SWS and waking groggy. Use an alarm to prevent oversleeping. A cup of coffee taken just before the nap can enhance wakening with energy as it takes about 30 to 40 minutes for the caffeine to be absorbed. |
| 30 to 60 minutes
SWS Sleep |
Generally, avoid naps of this duration; they result in waking during SWS sleep and grogginess which can last for 30 minutes. |
| 60 to 90 minutes
Full sleep cycle |
Allows a full sleep cycle and waking refreshed during stage1/REM sleep. Use an alarm set for 90 minutes, or use a smartphone app or another device that monitors motion and wakes the sleeper during the light, stage-1 sleep. Phone apps such as “Sleepbot,” “Sleep Cycle,” or “Sleep” may be used to monitor sleep at night. Some apps can even be used as screening tools for sleep disorders such as sleep apnea. |
A “power nap” lasting from six to 30 minutes provides mainly Stage 2 sleep; it is refreshing and improves motor skills and declarative memory[90],[91]. Shorter naps, less than 30 minutes, avoid sleep SWS and thus, avoid sleep inertia and grogginess upon awakening, which can last 30 minutes. Nevertheless, longer naps that include SWS provide more sustained cognitive performance than do short naps[92]. Napping for 60 to 90 minutes may allow an entire sleep cycle, thus allowing the napper to awakening from Stage 1/REM, refreshed without sleep inertia. A supine position is better than a seated position for napping[93]. (Sleeping supine increases the glymphatic flow and clearing of toxins from the brain.) It is best to avoid napping after four P.M. or within six hours of bedtime, to avoid disrupting the nighttime sleep cycle.
[1] Sleep deprivation: Impact on cognitive performance. Alhola P, Polo-Kantola P. Neuropsychiatr Dis Treat. 2007;3(5):553-67. PMID:19300585
[2] Fatigue, alcohol and performance impairment. Dawson D, Reid K. Nature. 1997 Jul 17;388(6639):235. PMID:9230429
[3] Does abnormal sleep impair memory consolidation in schizophrenia? Manoach DS, Stickgold R. Front Hum Neurosci. 2009 Sep 1;3:21. PMID:19750201
[4] Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Van Dongen HP, Baynard MD, Maislin G, Dinges DF. Sleep. 2004 May 1;27(3):423-33.PMID: 15164894
[5] The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. Sleep. 2003 Mar 15;26(2):117-26. PMID: 12683469
[6] Sleep drives metabolite clearance from the adult brain. Xie L, Kang H, Xu Q, et al. Science. 2013 Oct 18;342(6156):373-7. PMID:24136970
[7] Paradoxical sleep deprivation impairs spatial learning and affects membrane excitability and mitochondrial protein in the hippocampus.Yang RH, Hu SJ, Wang Y, Zhang WB, Luo WJ, Chen JY. Brain Res. 2008 Sep 16;1230:224-32. 18674519
[8] CLOCK and BMAL1 regulate MyoD and are necessary for maintenance of skeletal muscle phenotype and function.Andrews JL, Zhang X, McCarthy JJ, et al. Proc Natl Acad Sci U S A. 2010 Nov 2;107(44):19090-5. PMID: 20956306
[9] Why we sleep: the temporal organization of recovery. Mignot E. PLoS Biol. 2008 Apr 29;6(4):e106. PMID:18447584
[10] Melatonin signaling and cell protection function. Luchetti F, Canonico B, Betti M, et al. FASEB J. 2010 Oct;24(10):3603-24. PMID:20534884
[11] Sleep depth and fatigue: role of cellular inflammatory activation. Thomas KS, Motivala S, Olmstead R, Irwin MR. Brain Behav Immun. 2011 Jan;25(1):53-8..PMID: 20656013
[12] Retinoid-related orphan receptors (RORs): critical roles in development, immunity, circadian rhythm, and cellular metabolism. Jetten AM. Nucl Recept Signal. 2009;7:e003. PMID:19381306
[13] Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin.Spiegel K, Leproult R, L’hermite-Balériaux M, Copinschi G, Penev PD, Van Cauter E. J Clin Endocrinol Metab. 2004 Nov;89(11):5762-71.PMID: 15531540
[14] Sleep restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP.van Leeuwen WM, Lehto M, Karisola P, Lindholm H, et al. PLoS One. 2009;4(2):e4589. PMID: 19240794
[15] Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index.Taheri S, Lin L, Austin D, Young T, Mignot E. PLoS Med. 2004 Dec;1(3):e62. PMID: 15602591
[16] Polysomnographic sleep, growth hormone insulin-like growth factor-I axis, leptin, and weight loss.Rasmussen MH, Wildschiødtz G, Juul A, Hilsted J. Obesity (Silver Spring). 2008 Jul;16(7):1516-21. PMID: 18464752
[17] Improved prediction of all-cause mortality by a combination of serum total testosterone and insulin-like growth factor I in adult men.. Friedrich N, Schneider HJ, Haring R, et al. Steroids. 2012 Jan;77(1-2):52-8. PMID:22037276
[18] Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines.. Vgontzas AN, Zoumakis E, Bixler EO, Lin HM, Follett H, Kales A, Chrousos GP. J Clin Endocrinol Metab. 2004 May;89(5):2119-26.PMID: 15126529
[19] Effect of zinc and melatonin supplementation on cellular immunity in rats with toxoplasmosis. Baltaci AK, Bediz CS, Mogulkoc R, Kurtoglu E, Pekel A. Biol Trace Elem Res. 2003 Winter;96(1-3):237-45. PMID:14716103
[20] Meta-analysis of short sleep duration and obesity in children and adults. Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA. Sleep. 2008 May;31(5):619-26. PMID:18517032
[21] Increased risk of benign prostate hyperplasia in sleep apnea patients: a nationwide population-based study. Chou PS, Chang WC, Chou WP, et al. PLoS One. 2014 Mar 25;9(3):e93081. PMID:24667846
[22] Risk of Cancer in Patients with Insomnia, Parasomnia, and Obstructive Sleep Apnea: A Nationwide Nested Case-Control Study. Fang HF, Miao NF, Chen CD, Sithole T, Chung MH. J Cancer. 2015 Sep 15;6(11):1140-7. PMID:26516362
[23] Sleep apnea and the subsequent risk of breast cancer in women: a nationwide population-based cohort study. Chang WP, Liu ME, Chang WC, Yang AC, Ku YC, Pai JT, Lin YW, Tsai SJ. Sleep Med. 2014 Sep;15(9):1016-20. PMID:25085620
[24] Sleep apnea increased incidence of primary central nervous system cancers: a nationwide cohort study. Chen JC, Hwang JH. Sleep Med. 2014 Jul;15(7):749-54. PMID:24891080
[25] Night work, shift work: Breast cancer risk factor?. Benabu JC, Stoll F, Gonzalez M, Mathelin C. Gynecol Obstet Fertil. 2015 Dec;43(12):791-9. PMID:26597486
[26] Rotating night shifts and risk of breast cancer in women participating in the nurses’ health study. Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I, Colditz GA. J Natl Cancer Inst. 2001 Oct 17;93(20):1563-8. PMID:11604480
[27] A meta-analysis on dose-response relationship between night shift work and the risk of breast cancer. Wang F, Yeung KL, Chan WC, Kwok CC, Leung SL, Wu C, Chan EY, Yu IT, Yang XR, Tse LA. Ann Oncol. 2013 Nov;24(11):2724-32. PMID:23975662
[28] Work at night and breast cancer–report on evidence-based options for preventive actions. Bonde JP, Hansen J, Kolstad HA, et al. Scand J Work Environ Health. 2012 Jul;38(4):380-90. PMID:22349009
[29] Does night-shift work increase the risk of prostate cancer? a systematic review and meta-analysis. Rao D, Yu H, Bai Y, Zheng X, Xie L. Onco Targets Ther. 2015 Oct 5;8:2817-26. PMID:26491356
[30] A meta-analysis including dose-response relationship between night shift work and the risk of colorectal cancer. Wang X, Ji A, Zhu Y, Liang Z, Wu J, Li S, Meng S, Zheng X, Xie L. Oncotarget. 2015 Sep 22;6(28):25046-60. PMID:26208480
[31] Role of clock genes in gastrointestinal motility. Hoogerwerf WA. Am J Physiol Gastrointest Liver Physiol. 2010 Sep;299(3):G549-55. PMID:20558764
[32] Circadian variation in the propagation velocity of the migrating motor complex. Kumar D, Wingate D, Ruckebusch Y. Gastroenterology. 1986 Oct;91(4):926-30. PMID:3743969
[33] Melatonin and serotonin effects on gastrointestinal motility. Thor PJ, Krolczyk G, Gil K, Zurowski D, Nowak L. J Physiol Pharmacol. 2007 Dec;58 Suppl 6:97-103. PMID:18212403
[34] Functional bowel disorders in rotating shift nurses may be related to sleep disturbances.. Zhen Lu W, Ann Gwee K, Yu Ho K. Eur J Gastroenterol Hepatol. 2006 Jun;18(6):623-7. PMID:16702851
[35] Feeding cues alter clock gene oscillations and photic responses in the suprachiasmatic nuclei of mice exposed to a light/dark cycle. Mendoza J, Graff C, Dardente H, Pevet P, Challet E. J Neurosci. 2005 Feb 9;25(6):1514-22. PMID:15703405
[36] Restricted feeding uncouples circadian oscillators in peripheral tissues from the central pacemaker in the suprachiasmatic nucleus. Damiola F, Le Minh N, Preitner N, Kornmann B, Fleury-Olela F, Schibler U. Genes Dev. 2000 Dec 1;14(23):2950-61. PMID:11114885
[37] Effect of a phase advance and phase delay of the 24-h cycle on energy metabolism, appetite, and related hormones. Gonnissen HK, Rutters F, Mazuy C, Martens EA, Adam TC, Westerterp-Plantenga MS. Am J Clin Nutr. 2012 Oct;96(4):689-97. PMID:22914550
[38] Circadian aspects of postprandial metabolism. Morgan L, Hampton S, Gibbs M, Arendt J. Chronobiol Int. 2003 Sep;20(5):795-808. PMID:14535354
[39] The impact of the circadian timing system on cardiovascular and metabolic function. Morris CJ, Yang JN, Scheer FA. Prog Brain Res. 2012;199:337-58. PMID:22877674
[40] Dietary inflammatory index scores differ by shift work status: NHANES 2005 to 2010. Wirth MD, Burch J, Shivappa N, Steck SE, Hurley TG, Vena JE, Hébert JR. J Occup Environ Med. 2014 Feb;56(2):145-8. PMID:24451608
[41] Appetite-regulating hormones from the upper gut: disrupted control of xenin and ghrelin in night workers. Schiavo-Cardozo D, Lima MM, Pareja JC, Geloneze B. Clin Endocrinol (Oxf). 2012 Dec 1. PMID:23199168
[42] Total and cause-specific mortality of U.S. nurses working rotating night shifts. Gu F, Han J, Laden F, Pan A, et al. Am J Prev Med. 2015 Mar;48(3):241-52. PMID:25576495
[43] Shifting eating to the circadian rest phase misaligns the peripheral clocks with the master SCN clock and leads to a metabolic syndrome. Mukherji A, Kobiita A, Damara M, Misra N, Meziane H, Champy MF, Chambon P. Proc Natl Acad Sci U S A. 2015 Dec 1;112(48):E6691-8. PMID:26627260
[44] Alcohol use in shiftworkers. Dorrian J, Heath G, Sargent C, Banks S, Coates A. Accid Anal Prev. 2015 Nov 24. pii: S0001-4575(15)30127-5. PMID:26621201
[45] Rotating night-shift work and lung cancer risk among female nurses in the United States. Schernhammer ES, Feskanich D, Liang G, Han J. Am J Epidemiol. 2013 Nov 1;178(9):1434-41. PMID:24049158
[46] Breast cancer cells: Modulation by melatonin and the ubiquitin-proteasome system – A review. Vriend J, Reiter RJ. Mol Cell Endocrinol. 2015 Dec 5;417:1-9. PMID:26363225
[47] Light during darkness, melatonin suppression and cancer progression. Blask DE, Dauchy RT, Sauer LA, Krause JA, Brainard GC. Neuro Endocrinol Lett. 2002 Jul;23 Suppl 2:52-6. PMID:12163849
[48] Melatonin: an inhibitor of breast cancer. Hill SM, Belancio VP, Dauchy RT, et al. Endocr Relat Cancer. 2015 Jun;22(3):R183-204PMID:25876649
[49] Circadian and melatonin disruption by exposure to light at night drives intrinsic resistance to tamoxifen therapy in breast cancer. Dauchy RT, Xiang S, Mao L, et al. Cancer Res. 2014 Aug 1;74(15):4099-110. PMID:25062775
[50] Melatonin-depleted blood from premenopausal women exposed to light at night stimulates growth of human breast cancer xenografts in nude rats. Blask DE, Brainard GC, Dauchy RT, Hanifin JP, Davidson LK, Krause JA, Sauer LA, Rivera-Bermudez MA, Dubocovich ML, Jasser SA, Lynch DT, Rollag MD, Zalatan F. Cancer Res. 2005 Dec 1;65(23):11174-84. PMID: 16322268
[51] Predicting human nocturnal nonvisual responses to monochromatic and polychromatic light with a melanopsin photosensitivity function. Revell VL, Barrett DC, Schlangen LJ, Skene DJ. Chronobiol Int. 2010 Oct;27(9-10):1762-77. doi: 10.3109/07420528.2010.516048. PMID:20969522
[52] Dim light during darkness stimulates tumor progression by enhancing tumor fatty acid uptake and metabolism. Dauchy RT, Blask DE, Sauer LA, Brainard GC, Krause JA. Cancer Lett. 1999 Oct 1;144(2):131-6. PMID:10529012
[53] Work at night and breast cancer–report on evidence-based options for preventive actions. Bonde JP, Hansen J, Kolstad HA, et al. Scand J Work Environ Health. 2012 Jul;38(4):380-90. PMID:22349009
[54] Daytime Blue Light Enhances the Nighttime Circadian Melatonin Inhibition of Human Prostate Cancer Growth. Dauchy RT, Hoffman AE, Wren-Dail MA, Hanifin JP, Warfield B, Brainard GC, Xiang S, Yuan L, Hill SM, Belancio VP, Dauchy EM, Smith K, Blask DE. Comp Med. 2015;65(6):473-85. PMID:26678364
[55] The potential role of the transcription factor RZR/ROR as a mediator of nuclear melatonin signaling. Wiesenberg I, Missbach M, Carlberg C. Restor Neurol Neurosci. 1998 Jun;12(2-3):143-50. PMID:12671309
[56] RORα and ROR γ are expressed in human skin and serve as receptors for endogenously produced noncalcemic 20-hydroxy- and 20,23-dihydroxyvitamin D. Slominski AT, Kim TK, Takeda Y, Janjetovic Z, Brozyna AA, Skobowiat C, Wang J, Postlethwaite A, Li W, Tuckey RC, Jetten AM. FASEB J. 2014 Jul;28(7):2775-89. PMID:24668754
[57] Vitamin B12 enhances the phase-response of circadian melatonin rhythm to a single bright light exposure in humans. Hashimoto S, Kohsaka M, Morita N, Fukuda N, Honma S, Honma K. Neurosci Lett. 1996 Dec 13;220(2):129-32.PMID: 8981490
[58] A multicenter study of sleep-wake rhythm disorders: therapeutic effects of vitamin B12, bright light therapy, chronotherapy and hypnotics. Yamadera H, Takahashi K, Okawa M. Psychiatry Clin Neurosci. 1996 Aug;50(4):203-9. PMID:9201777
[59] Sleep Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep. 2008 Aug 1;31(8):1087-96.PMID: 18714780
[60] Mortality associated with sleep duration and insomnia. Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Arch Gen Psychiatry. 2002 Feb;59(2):131-6.PMID: 11825133
[61] Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Chien KL, Chen PC, Hsu HC, Su TC, Sung FC, Chen MF, Lee YT. Sleep. 2010 Feb 1;33(2):177-84.PMID: 20175401
[62] Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A; JACC Study Group. Sleep. 2009 Mar 1;32(3):295-301.PMID: 19294949
[63] Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep. 2010 May 1;33(5):585-92. PMID: 20469800
[64] Melatonin decreases delirium in elderly patients: a randomized, placebo-controlled trial. Al-Aama T, Brymer C, Gutmanis I, Woolmore-Goodwin SM, Esbaugh J, Dasgupta M. Int J Geriatr Psychiatry. 2010 Sep 15. PMID: 20845391
[65] Vitamin B6 and risk of colorectal cancer: a meta-analysis of prospective studies. Larsson SC, Orsini N, Wolk A. JAMA. 2010 Mar 17;303(11):1077-83. PMID:20233826
[66] Melatonin improves metabolic syndrome induced by high fructose intake in rats.. Kitagawa A, Ohta Y, Ohashi K. J Pineal Res. 2011 Dec 7. PMID:22220562
[67] Clinical uses of melatonin: evaluation of human trials. Sánchez-Barceló EJ, Mediavilla MD, Tan DX, Reiter RJ. Curr Med Chem. 2010;17(19):2070-95. PMID:20423309
[68] The potential therapeutic effect of melatonin in Gastro-Esophageal Reflux Disease. Kandil TS, Mousa AA, El-Gendy AA, Abbas AM. BMC Gastroenterol. 2010 Jan 18;10:7. PMID:20082715
[69] The therapeutic potential of melatonin in migraines and other headache types. Gagnier JJ. Altern Med Rev. 2001 Aug;6(4):383-9. PMID:11578254
[70] Potential therapeutic use of melatonin in migraine and other headache disorders. Peres MF, Masruha MR, Zukerman E, Moreira-Filho CA, Cavalheiro EA. Expert Opin Investig Drugs. 2006 Apr;15(4):367-75. PMID:16548786
[71] The association of nocturnal serum melatonin levels with major depression in patients with acute multiple sclerosis. Akpinar Z, Tokgöz S, Gökbel H, Okudan N, Uğuz F, Yilmaz G. Psychiatry Res. 2008 Nov 30;161(2):253-7. PMID:18848732
[72] Optimal serum 25-hydroxyvitamin D levels for multiple health outcomes. Bischoff-Ferrari HA. Adv Exp Med Biol. 2008;624:55-71. PMID:18348447
[73] The effect of vitamin D supplements on the severity of restless legs syndrome. Wali S, Shukr A, Boudal A, Alsaiari A, Krayem A. Sleep Breath. 2015 May;19(2):579-83. PMID:25148866
[74] Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. Chowdhury R, Kunutsor S, Vitezova A, et al. BMJ. 2014 Apr 1;348:g1903. PMID:24690623
[75] Serum 25-hydroxyvitamin D, mortality, and incident cardiovascular disease, respiratory disease, cancers, and fractures: a 13-y prospective population study. Khaw KT, Luben R, Wareham N. Am J Clin Nutr. 2014 Nov;100(5):1361-70. PMID:25332334
[76] Cognitive impairment associated with low ferritin responsive to iron supplementation. Qubty W, Renaud DL. Pediatr Neurol. 2014 Dec;51(6):831-3. PMID:25283751
[77] Children with autism: effect of iron supplementation on sleep and ferritin. Dosman CF, Brian JA, Drmic IE, Senthilselvan A, Harford MM, Smith RW, Sharieff W, Zlotkin SH, Moldofsky H, Roberts SW. Pediatr Neurol. 2007 Mar;36(3):152-8.PMID: 17352947
[78] Improvement of anemia with erythropoietin and intravenous iron reduces sleep-related breathing disorders and improves daytime sleepiness in anemic patients with congestive heart failure. Zilberman M, Silverberg DS, Bits I, et al. Am Heart J. 2007 Nov;154(5):870-6. PMID: 17967592
[79] Diagnostic accuracy of behavioral, activity, ferritin, and clinical indicators of restless legs syndrome. Richards KC, Bost JE, Rogers VE, Hutchison LC, Beck CK, Bliwise DL, Kovach CR, Cuellar N, Allen RP. Sleep. 2015 Mar 1;38(3):371-80. PMID:25325464
[80] Iron deficiency and infant motor development.. Shafir T, Angulo-Barroso R, Jing Y, et al. Early Hum Dev. 2008 Jul;84(7):479-85. PMID: 18272298
[81] Dietary intake of B vitamins and methionine and colorectal cancer risk. Bassett JK, Severi G, Hodge AM, Baglietto L, Hopper JL, English DR, Giles GG. Nutr Cancer. 2013;65(5):659-67. PMID:23859033
[82] Acute ethanol modulates glutamatergic and serotonergic phase shifts of the mouse circadian clock in vitro. Prosser RA, Mangrum CA, Glass JD. Neuroscience. 2008 Mar 27;152(3):837-48. PMID: 18313277
[83] Habitual moderate alcohol consumption desynchronizes circadian physiologic rhythms and affects reaction-time performance. Reinberg A, Touitou Y, Lewy H, Mechkouri M. Chronobiol Int. 2010 Oct.;27(9-10):1930-1942.PMID: 20969532
[84] Circadian rhythm of hormones is extinguished during prolonged physical stress, sleep and energy deficiency in young men.. Opstad K. Eur J Endocrinol. 1994 Jul;131(1):56-66.PMID: 8038905
[85] High intention to fall asleep causes sleep fragmentation. Rasskazova E, Zavalko I, Tkhostov A, Dorohov V. J Sleep Res. 2014 Jun;23(3):295-301. PMID:24387832
[86] Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Chang AM, Aeschbach D, Duffy JF, Czeisler CA. Proc Natl Acad Sci U S A. 2015 Jan 27;112(4):1232-7. PMID:25535358
[87] Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. van der Lely S, Frey S, Garbazza C, Wirz-Justice A, Jenni OG, Steiner R, Wolf S, Cajochen C, Bromundt V, Schmidt C. J Adolesc Health. 2015 Jan;56(1):113-9. PMID:25287985
[88] Bigger, Brighter, Bluer-Better? Current Light-Emitting Devices – Adverse Sleep Properties and Preventative Strategies. Gringras P, Middleton B, Skene DJ, Revell VL. Front Public Health. 2015 Oct 13;3:233. PMID:26528465
[89] Daytime napping after a night of sleep loss decreases sleepiness, improves performance, and causes beneficial changes in cortisol and interleukin-6 secretion. Vgontzas AN, Pejovic S, Zoumakis E, et al. Am J Physiol Endocrinol Metab. 2007 Jan;292(1):E253-61.PMID: 16940468
[90] The impact of sleep duration and subject intelligence on declarative and motor memory performance: how much is enough? Tucker MA, Fishbein W. J Sleep Res. 2009 Sep;18(3):304-12. PMID:19702788
[91] Enhancement of declarative memory performance following a daytime nap is contingent on strength of initial task acquisition. Tucker MA, Fishbein W. Sleep. 2008 Feb;31(2):197-203. PMID:18274266
[92] Post-sleep inertia performance benefits of longer naps in simulated nightwork and extended operations. Mulrine HM, Signal TL, van den Berg MJ, Gander PH. Chronobiol Int. 2012 Nov;29(9):1249-57. PMID:23002951
[93] Effects of physical positions on sleep architectures and post-nap functions among habitual nappers. Zhao D, Zhang Q, Fu M, Tang Y, Zhao Y. Biol Psychol. 2010 Mar;83(3):207-13. PMID:20064578